58M generalised weakness
A 58 yr old male with generalised weakness
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
Chief complaints
A 58 yr old male was bought to the casualty with the complaints of generalised weakness and fatigue.
History of presenting illness
The patient was apparently asymptomatic 30 yrs ago then he started drinking toddy 1 bottle in evening after doing agriculture work . He continued drinking toddy for next 10 yrs . Later the patient shifted to drinking liquor half bottle initially almost 2-3 times in a week. He then experienced sleep disturbances, sweating, palpitations, mild tremors, if he stopped drinking for 1 day. He was currently drinking 500ml of liquor since past 1 month. He developed generalized weakness easy fatiguibility, giddiness 1 week ago. Hence got admitted in private hospital in miryalguda. He developed hypotension and was in unresponsive state hence in emergency shifted to Kim's hospital. He was having occasional irreleavent talk.
Past history
No history of hypertension, diabetes mellitus, TB , CAD , CVA , epilepsy, thyroid, asthma.
Personal history
Mixed diet
Sleep irregular since 5 days
Appetite decreased
Bowel and bladder regular
Addiction: alochol since 30 yrs
Smoking(5-6 beedis a day)
Family history
Not significant
General examination
Patient is examined in a well lit room after taking an informed consent.
Patient is conscious and coherent.
No signs of pallor, icterus, clubbing, cyanosis, generalized lymphadenopathy, pedal edema.
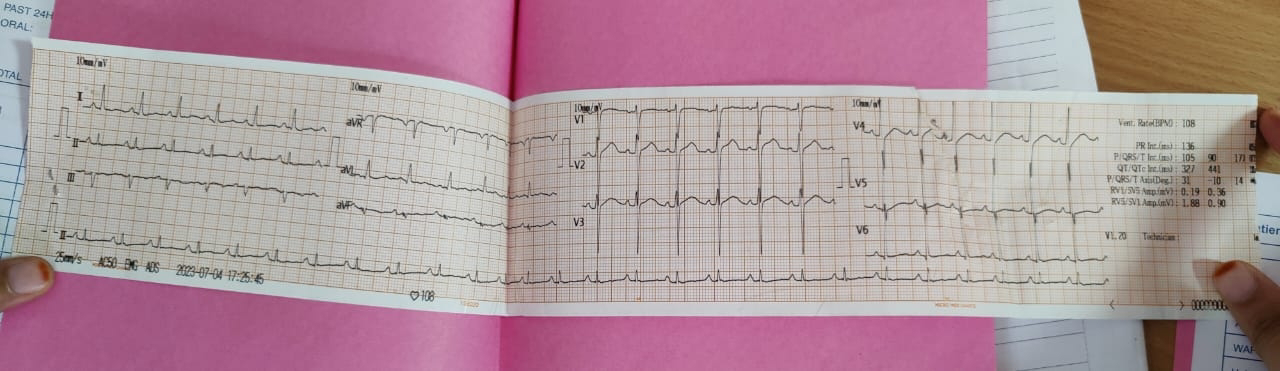
Vitals
Temperature:98.6F
Pulse rate: 106 per min
RR :18/min
BP :80/40 mmof Hg
SpO2:98%
Systemic examination
CVS: S1,S2 heard , no murmurs
RS: BLAE(benign lymphangioendothelioma ) present
P/A: SOFT, NON TENDER
CNS: NO FOCAL DEFICITS
Provisional diagnosis
Hypovolaemic shock.









Comments
Post a Comment